Azithromycin is thought to be a nice choice for the treatment of respiratory infections because it covers atypical pathogens, has favorable pharmacokinetics, and also anti-inflammatory properties. Its use is widespread in conditions such as bronchitis, community-acquired pneumonia, and chronic obstructive pulmonary disease (COPD) exacerbations. It has worked in clinical trials, curing over 85% of bacterial respiratory infections caused by common pathogens like Streptococcus pneumoniae and Haemophilus influenzae.
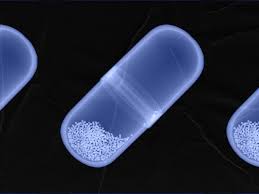
The single-largest advantage of using azithromycin as treatment for respiratory infections lies in its ability to achieve substantial tissue concentration. Its half-life is approximately 68 hours, allowing it to maintain high levels within lung and sinus tissue for several days after the last dose. This makes it particularly effective in short-course therapies, such as a five-day regimen where 500 mg is administered on the first day followed by 250 mg daily for the next four days. Evidence suggests this regimen is bactericidal for common respiratory pathogens, achieving over 90% eradication rates.
Azithromycin’s mechanism of action as a macrolide antibiotic involves binding to the 50S subunit of bacterial ribosomes, inhibiting RNA-dependent protein synthesis and thereby disrupting bacterial accumulation. Its effectiveness against both typical and atypical respiratory pathogens, such as Mycoplasma pneumoniae and Legionella pneumophila, reinforces its role as a first-line therapy for community-acquired pneumonia when atypical pathogens are suspected.
In addition to its antibacterial properties, azithromycin’s anti-inflammatory effects provide an added benefit in managing respiratory disorders. The drug reduces pro-inflammatory cytokines, which aids in symptom management for chronic respiratory diseases. A clinical trial published in The Lancet last month showed that long-term azithromycin treatment reduced the risk of further acute exacerbations by 35%. Azithromycin’s dual action, combining antibacterial and anti-inflammatory mechanisms, makes it particularly effective in treating infections where inflammation is a significant factor.
However, not all respiratory infections benefit from azithromycin. The rise in antibiotic-resistant strains has increased concerns about overprescribing. According to a CDC report, 30% of outpatient antibiotic prescriptions in the U.S. are unnecessary, and azithromycin is among the commonly overused medications. Overuse leads to resistance, diminishing the drug’s effectiveness over time. Clinicians must carefully evaluate when azithromycin is truly beneficial based on the specific pathogen and the patient’s medical history.
Regarding side effects and contraindications, the FDA has issued warnings about the risk of QT interval prolongation, which can lead to life-threatening arrhythmias. Although rare, patients should be closely monitored for up to 10 days after taking azithromycin, especially those with a history of heart disease or those taking other QT-prolonging medications. Despite these risks, azithromycin remains a valuable treatment option, particularly when its benefits outweigh its relative risks.
Azithromycin’s suitability for a wide variety of respiratory infections is largely due to its broad-spectrum bactericidal activity, high tissue penetration, and multiple anti-inflammatory effects. When used correctly, it serves as a crucial resource for treating conditions like pneumonia and COPD exacerbations. Understanding these key aspects further highlights what is azithromycin used for and reinforces its relevance in modern medicine.